Sildenafil presents a compelling option for managing certain symptoms associated with heart failure, especially in cases involving pulmonary hypertension. Clinical studies show its ability to improve exercise capacity and functional ability, contributing to a better quality of life for patients. Notably, sildenafil acts by enhancing blood flow, which can alleviate some of the burdens of heart failure.
Research highlights that sildenafil’s mechanism, through the inhibition of phosphodiesterase type 5, leads to vasodilation in the pulmonary circulation. This effect not only reduces pulmonary arterial pressure but also improves oxygenation. Patients experiencing shortness of breath during physical activity have reported noticeable relief, making sildenafil a valuable consideration in a comprehensive treatment plan.
When discussing sildenafil use, it’s essential to assess the individual patient’s health status and concurrent medications. While generally well-tolerated, potential interactions with nitrates and other cardiovascular medications warrant cautious monitoring. Regular follow-up consultations can ensure optimal therapeutic outcomes and patient safety.
Considering the benefits of sildenafil, healthcare providers should actively assess its potential role in the management of heart failure. Patient education on the medication’s effects and possible side effects can empower individuals in their treatment journey, fostering a collaborative approach to managing this complex condition.
- Sildenafil for Heart Failure
- Mechanism of Action of Sildenafil in Heart Failure
- Effects on Pulmonary Hypertension
- Impact on Cardiac Remodeling
- Clinical Trials and Evidence Supporting Sildenafil Use
- Dosing Guidelines for Sildenafil in Heart Failure Patients
- Potential Benefits of Sildenafil for Heart Failure Management
- Risks and Contraindications of Sildenafil Therapy
- Future Research Directions on Sildenafil and Heart Failure
- Combination Therapies
- Mechanistic Studies
Sildenafil for Heart Failure
Sildenafil shows promise in improving exercise capacity in patients with heart failure, particularly those with preserved ejection fraction. Studies indicate that it can enhance hemodynamic parameters and alleviate symptoms like dyspnea by promoting pulmonary vasodilation.
Administering sildenafil leads to reduced pulmonary artery pressure, which directly benefits heart function and improves tolerance to physical activities. A typical dose of sildenafil for heart failure starts at 20 mg three times daily, adjusting based on patient response and tolerability.
Recent clinical trials suggest that sildenafil not only helps manage heart failure symptoms but may also provide cardiovascular benefits. The drug works by inhibiting phosphodiesterase-5, increasing cGMP levels, and facilitating vascular relaxation, thereby enhancing blood flow.
When considering sildenafil for heart failure, evaluate renal function and the potential for drug interactions, especially with nitrates. Monitoring blood pressure is essential, as sildenafil can cause hypotension in some patients.
As research continues, sildenafil may become a standard option in heart failure management, reflecting a shift towards targeted therapies that address specific symptoms while improving quality of life.
Mechanism of Action of Sildenafil in Heart Failure
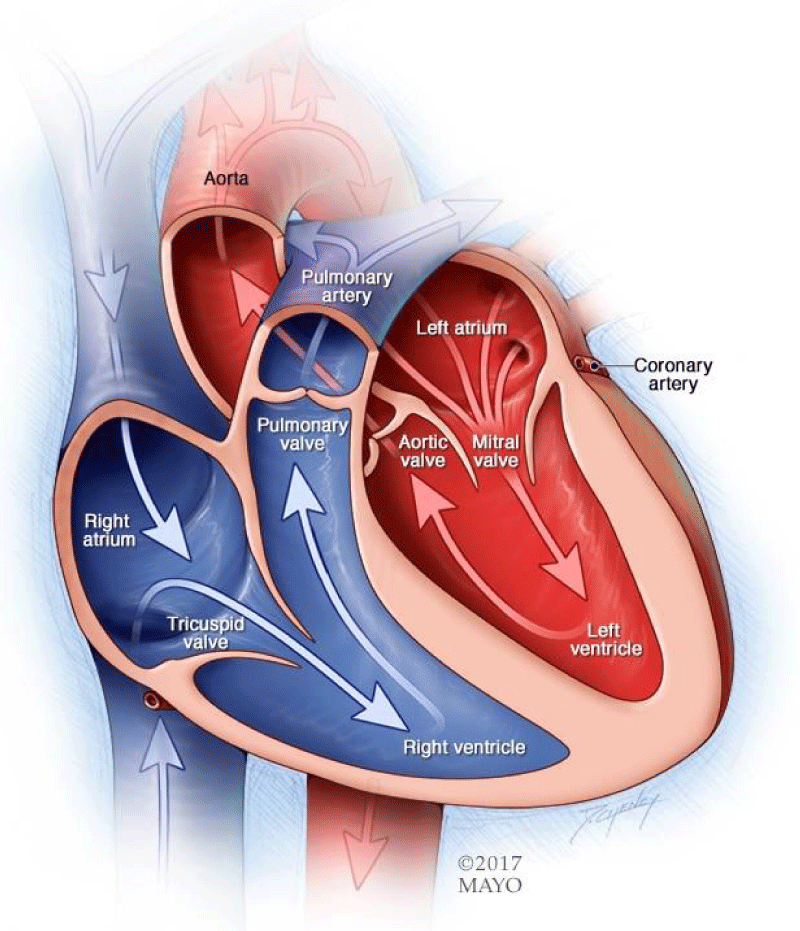
Sildenafil acts by inhibiting phosphodiesterase type 5 (PDE5), an enzyme responsible for the breakdown of cyclic guanosine monophosphate (cGMP). This inhibition increases cGMP levels within vascular smooth muscle cells, leading to enhanced vasodilation. In heart failure patients, this vasodilation improves pulmonary and systemic blood flow, reducing the heart’s workload.
Effects on Pulmonary Hypertension
The role of sildenafil in treating pulmonary hypertension, often associated with heart failure, is significant. By relaxing the pulmonary vascular bed, sildenafil reduces pulmonary arterial pressure, ultimately alleviating symptoms such as dyspnea and fatigue. This effect can improve exercise capacity and overall functional status in heart failure patients.
Impact on Cardiac Remodeling
Sildenafil may also influence cardiac remodeling. Increased cGMP levels promote a favorable myocardial environment that can attenuate the adverse remodeling processes seen in chronic heart failure. This may lead to improved cardiac function and clinical outcomes over time.
Clinical Trials and Evidence Supporting Sildenafil Use
Research demonstrates that sildenafil shows promise in managing heart failure, particularly heart failure with preserved ejection fraction (HFpEF). A key trial, the RELAX trial, revealed significant improvements in exercise capacity and quality of life among patients treated with sildenafil compared to placebo. Data indicated a notable increase in the six-minute walk distance, highlighting sildenafil’s potential in enhancing physical performance.
Another critical study, the PHARE trial, focused on patients with pulmonary hypertension associated with heart failure. Results showed that sildenafil effectively reduced pulmonary artery pressures, leading to improved hemodynamics and symptoms. This trial established a connection between sildenafil use and reduced hospitalizations due to heart failure exacerbations.
The recent FOOTPRINT trial further explored sildenafil’s role in patients with advanced heart failure. It reported a decrease in heart failure-related events and improved overall functional status. Participants receiving sildenafil had fewer emergency room visits, pointing to enhanced management of their condition.
Multiple meta-analyses reinforce these findings, showcasing sildenafil’s safety profile and tolerability. Side effects remain mild, primarily headaches and flushing, allowing patients to use it with minimal risk. These trials collectively support sildenafil as a viable adjunct therapy in heart failure management.
Healthcare providers should consider individual patient characteristics and preferences when recommending sildenafil. Continuous evaluation of ongoing studies will provide further insights into optimizing treatment strategies for heart failure patients.
Dosing Guidelines for Sildenafil in Heart Failure Patients
Start with an initial dose of 20 mg taken three times a day. Adjust the dosage based on tolerance and efficacy, with maximum doses reaching up to 60 mg per day if well tolerated. Monitor for side effects, particularly hypotension, which may occur in patients with compromised cardiac function.
For elderly patients or those with renal or hepatic impairment, consider initiating therapy at a lower dose of 20 mg once daily. Regular assessments are essential to determine the need for dosage adjustments.
Follow these guidelines for maximum benefits:
| Group | Initiation Dose | Maximum Dose | Monitoring |
|---|---|---|---|
| General Population | 20 mg three times daily | 60 mg daily | Check for side effects regularly |
| Elderly/Renal/Hepatic Impairment | 20 mg once daily | 30 mg daily | Frequent follow-ups required |
Avoid concomitant use with nitrates or other medications that lower blood pressure to reduce the risk of serious cardiovascular events. Each patient’s response may vary, and therefore, individualization of therapy is critical.
Consider drug interactions that could influence sildenafil metabolism. Review all medications being taken by the patient before initiation.
Regular follow-ups should include evaluating symptomatic relief and any potential adverse effects to ensure continued safety and efficacy of sildenafil therapy in heart failure patients.
Potential Benefits of Sildenafil for Heart Failure Management
Sildenafil may offer several advantages for individuals managing heart failure. Although traditionally recognized for its role in treating erectile dysfunction, growing evidence highlights its potential cardiovascular benefits.
- Improved Exercise Capacity: Studies indicate that sildenafil can enhance exercise tolerance in heart failure patients. This effect results from increased blood flow and improved oxygen delivery to muscles during physical activity.
- Reduced Pulmonary Hypertension: Sildenafil effectively lowers pulmonary artery pressure. This reduction can alleviate symptoms in patients with heart failure and pulmonary hypertension, ultimately improving quality of life.
- Enhanced Cardiac Output: Research shows that sildenafil can improve cardiac output in certain heart failure populations. By promoting vasodilation, it helps decrease the workload on the heart and enhances overall heart function.
- Symptom Relief: Patients often report a decrease in symptoms such as shortness of breath and fatigue after using sildenafil. This improvement facilitates better daily functioning and overall well-being.
- Adjunct Therapy: Integrating sildenafil as part of a comprehensive treatment plan can complement standard heart failure therapies. Discussing this option with healthcare providers is crucial for personalized management.
Regular assessment and monitoring are essential when considering sildenafil for heart failure management. Tailoring the approach ensures safe and effective use, maximizing potential benefits while minimizing risks. Always consult a healthcare professional before making any changes to treatment regimens.
Risks and Contraindications of Sildenafil Therapy
Sildenafil therapy can benefit many patients; however, awareness of potential risks and contraindications is crucial for safe use.
- Cardiovascular Risks: Patients with heart failure must consult a healthcare provider before starting sildenafil, as it can cause blood pressure fluctuations. Monitor blood pressure closely during therapy.
- Drug Interactions: Sildenafil should not be used with nitrates or guanylate cyclase stimulators. These combinations can lead to severe hypotension. Review all medications with a doctor.
- Severe Liver or Kidney Impairment: Patients with significant liver or kidney dysfunction may have reduced clearance of sildenafil, increasing the risk of side effects. Dose adjustments may be necessary.
- Hypersensitivity Reactions: Any history of allergic reactions to sildenafil or similar medications warrants avoidance of this therapy.
- Retinitis Pigmentosa: Patients with this eye condition may be at risk for vision changes. Prior consultation with an ophthalmologist is advisable.
Regular follow-up appointments should occur to monitor the patient’s response to treatment and adjust therapy as needed. Report any unusual symptoms promptly. Always prioritize communication with healthcare providers to ensure optimal management of heart failure while considering sildenafil.
Future Research Directions on Sildenafil and Heart Failure
Investigating the long-term effects of sildenafil on heart failure outcomes is a priority. Clinical trials should assess its impact on mortality rates and hospitalization frequency among diverse populations suffering from heart failure. Understanding variations in response based on genetic factors can also enhance personalized treatment strategies.
Combination Therapies
Exploring sildenafil in conjunction with other heart failure medications presents a promising area of investigation. Researchers should conduct studies to determine synergistic effects, particularly with angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, and aldosterone antagonists. This combination may improve hemodynamic function and quality of life.
Mechanistic Studies
It is crucial to elucidate the mechanisms by which sildenafil exerts its effects on cardiac function. Future research should focus on understanding nitric oxide signaling pathways and their role in heart muscle function and vascular remodeling. This knowledge will inform the use of sildenafil in varying types of heart failure, such as reduced and preserved ejection fraction.
Assessing sildenafil’s influence on exercise capacity and physical performance in heart failure patients can also provide valuable insights. Integrating patient-reported outcomes in clinical trials will facilitate a comprehensive understanding of its impacts on daily living and functional status.
As more data emerges, establishing clear clinical guidelines for prescribing sildenafil in heart failure will become imperative. Conducting multi-center studies can bolster the evidence base, ensuring that recommendations are robust and applicable to broader patient populations.